What is compression of the ulnar nerve at the elbow ?
In the normal state, the ulnar nerve passes through a pseudo-canal at the elbow. Any limitation of the ulnar nerve motion will cause abnormal traction, which causes the nerve to suffer.
The dynamic anatomy of the parietal elbow during the motion from extension to flexion is partly responsible for the suffering of the ulnar nerve in the long course.
Finally, the chronic instability of the ulnar nerve may be responsible for nerve suffering, by a repetitive conflict with the medial epicondyle.
The usual compressions of the ulnar nerve occurs at the fibrous muscular arch, or Osborne fascia. This fascia is located at the end of the side which corresponds to a thickening of the envelopes of the anterior ulnar muscle.
What are the clinical signs ?
Paresthesias in or numbness on the palmar side , the 4th and 5th fingers are the most common motives behind consultation. They may be associated with a weakness of the hand.
The clinician will then seek the set of sought clinical signs that reflect motor impairment: the Wartenberg sign which corresponds to the impossibility of bringing the little finger in contact with the other fingers (permanent abduction of the 5th finger), the Froment’s sign (weakness of the adductor and the deep bundle of the flexor), a muscular loss of the first interosseous space, a flattening of the hand with intermetacarpal atrophy of claws of the 4th and 5th fingers that can or can’t be reduced .
The clinical examination will end by seeking a chronic symptoms of ulnar nerve dislocation : from flexion to extension, the ulnar nerve is dislocated at the epitrochleo-olecranon gutter and passes forward of the medial epicondyle. This phenomenon is visible and palpable.
What other additional examination that should I have ?
An electromyogram that confirms the impaired sensory conduction and the slowing of the motor conduction at the elbow and an alteration of the recordings of the intrinsic muscles.
Simple x-rays of the elbow that can be used to diagnose bone damage.
What is the treatment ?
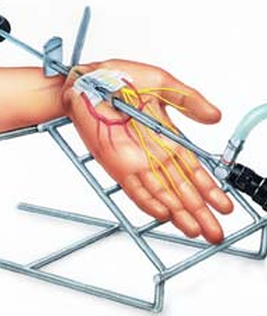
The treatment usually requires a surgy. It can be performed as an outpatient or during a short hospital stay of 1 to 2 nights, under loco-regional anesthesia.
The aim of the treatment is to perform a ulnar nerve decompression (neurolysis) by removing the causes of compression.
An anterior transposition of the nerve is also performed in the advanced motions. In case of transposition, the arm is immobilized in a splint for ten days.
There is a quick recovery of the sensory forms with almost immediate disappearance of paresthesias.
In acute forms of compression accompanied by hand amyotrophy, the disappearance of tingling is slower, and motion recovery takes several months.
Post-operative :
The neurolysis of the ulnar nerve is a surgey aiming to release the nerve from the arches compressing it at the level of the elbow.
The surgery allows at least to stop the evolution of paralysis and the loss of sensitivity, at best it allows the neurological recovery, and thus recovery of the contraction of the hand muscle and the sensitivity of the ring finger and the little finger.
The surgical treatment of the
ulnar nerve compression requires a fairly long recovery time (3 to 12 months).
The final result of decompression can not be assessed before one year after surgery, time required for the nerve to regenerate.
There two types of surgeries :
In Situ neurolysis :
Pure sensitive expression of the compression with stable nerve in its groove.
Often no immobilization is required.
Suitable analgesics are prescribed. A sick leave is often necessary for a few weeks.
A nurse should make your dressing every 4 days.
The first post-operative medical examination occurs at the end of the first week.
Neurolysis/ anterior subcutaneous transportation
Electromyographic motion expression or clinical expression or sensory expression on an unstable nerve or an impaired axis of the elbow.
An elbow splint is made in position of motion during the period of of healing (15 days).
Suitable analgesics are prescribed. A sick leave is often necessary for a few weeks.
Physiotherapy sessions may be required to overcome the motion deficit associated with the history of the nerve compression, the time for muscle recovery.